Table of Contents
Definition / general | Essential features | Terminology | ICD coding | Epidemiology | Sites | Pathophysiology | Etiology | Clinical features | Diagnosis | Radiology description | Radiology images | Prognostic factors | Case reports | Treatment | Gross description | Frozen section description | Microscopic (histologic) description | Microscopic (histologic) images | Positive stains | Negative stains | Sample pathology report | Differential diagnosis | Additional references | Board review style question #1 | Board review style answer #1 | Board review style question #2 | Board review style answer #2Cite this page: Lott Limbach A. Condensing osteitis. PathologyOutlines.com website. https://www.pathologyoutlines.com/topic/mandiblemaxillacondensingosteitis.html. Accessed April 30th, 2024.
Definition / general
- An area of sclerotic bone related to chronic osteomyelitis that is present at root of tooth (J Mass Dent Soc 2003;52:52)
- Tooth often demonstrates pulpitis or pulpal necrosis or previous restoration (J Mass Dent Soc 2003;52:52, J Endod 2013;39:977)
Essential features
- Dense sclerotic bone, seen radiographically, in area of a tooth with pulpitis or previous restoration
- Lesion resolves with treatment of affected tooth
Terminology
- Focal sclerosing osteomyelitis (J Mass Dent Soc 2003;52:52)
ICD coding
- ICD-10: M27.2 - inflammatory conditions of jaws
Epidemiology
- 4 - 7% of population (J Endod 2013;39:977)
- Early adolescence / young adults but can be any age (J Mass Dent Soc 2003;52:52)
- Mandible more frequently than maxilla (J Mass Dent Soc 2003;52:52)
Sites
- Oral cavity, mandible or maxilla, root of tooth (J Endod 2013;39:977)
Pathophysiology
- Related to chronic inflammation of pulp of tooth causing sclerotic bone formation (J Mass Dent Soc 2003;52:52)
Etiology
- Longstanding or low intensity infection with chronic inflammation and trabecular bone formation (J Mass Dent Soc 2003;52:52, J Endod 2013;39:977)
Clinical features
- Only clinical finding may be degenerative pulp disease (J Endod 2013;39:977)
Diagnosis
- Diagnosis made by imaging of jaw
Radiology description
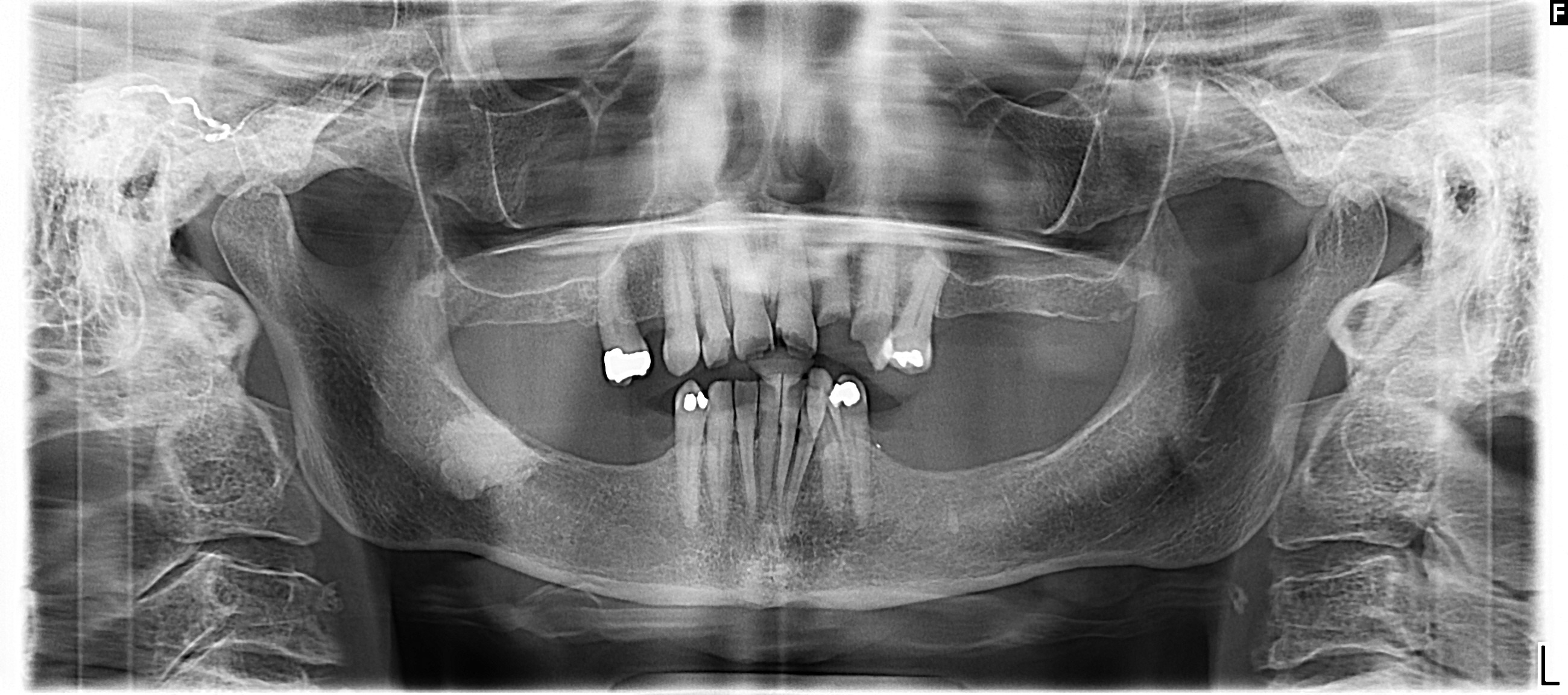
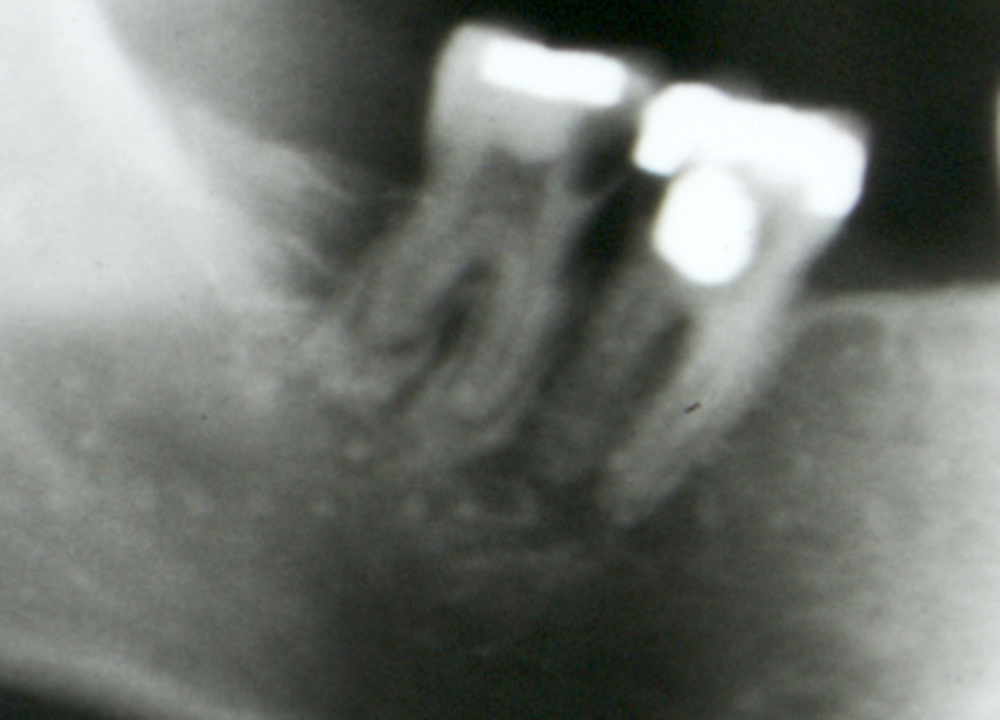
- Diffuse radiopaque borders concentrically arranged around root apex (J Endod 2013;39:977)
Radiology images
Prognostic factors
- Most regress after treatment of affected tooth
Case reports
- 23 year old woman, 27 year old man and 32 year old woman with radiopaque apical lesions (Bratisl Lek Listy 2009;110:713)
- 28 year old man with radiopaque lesion on routine imaging (Tex Dent J 2003;120:178)
- 57 year old woman with pain in right maxillary anterior region after extraction of upper left incisor (J Mass Dent Soc 2003;52:52)
Treatment
- Treatment of infection in affected tooth with hopeful regression after root canal therapy or extraction (J Mass Dent Soc 2003;52:52)
Gross description
- Bone, often fragmented
Frozen section description
- Frozen section not performed
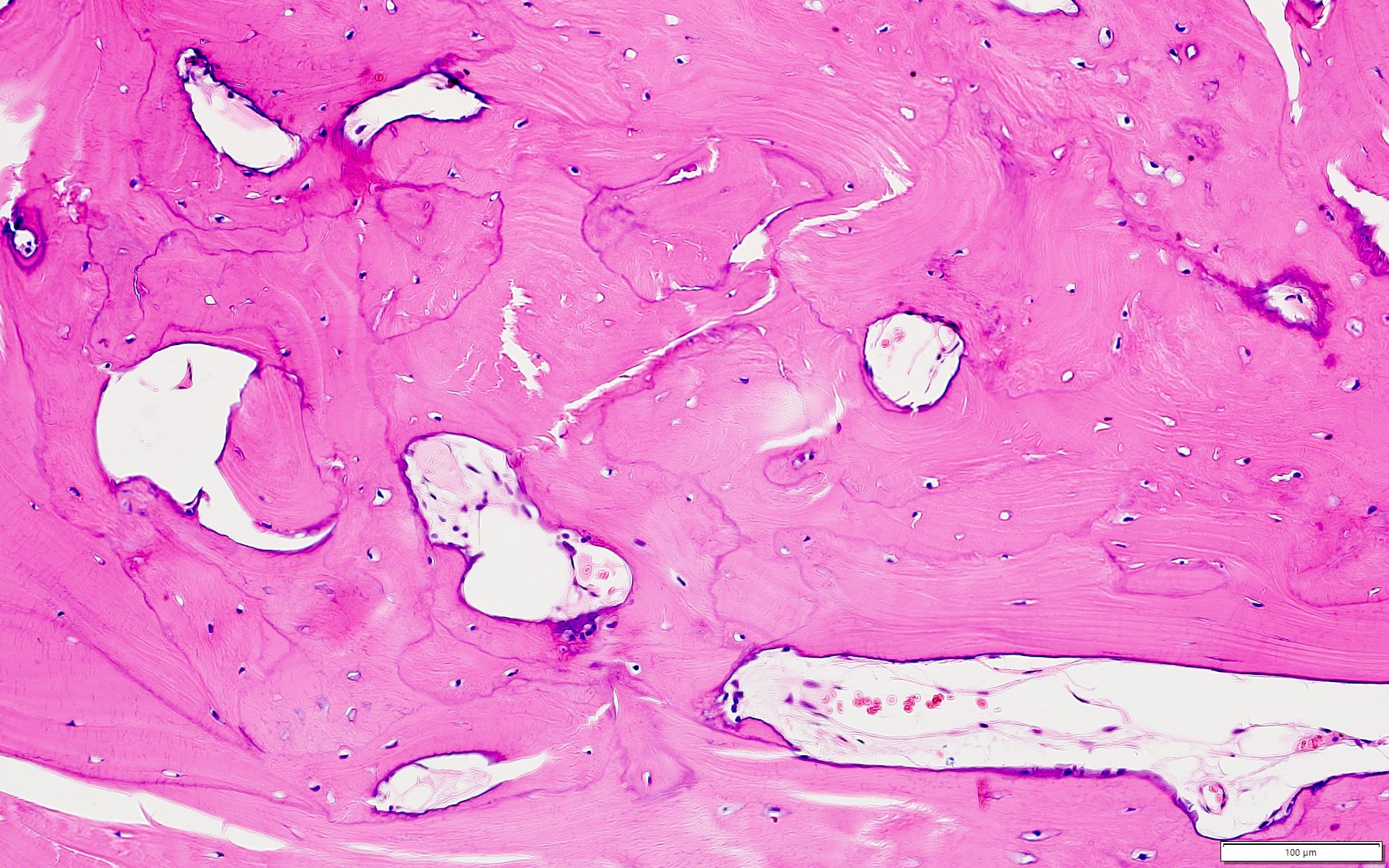
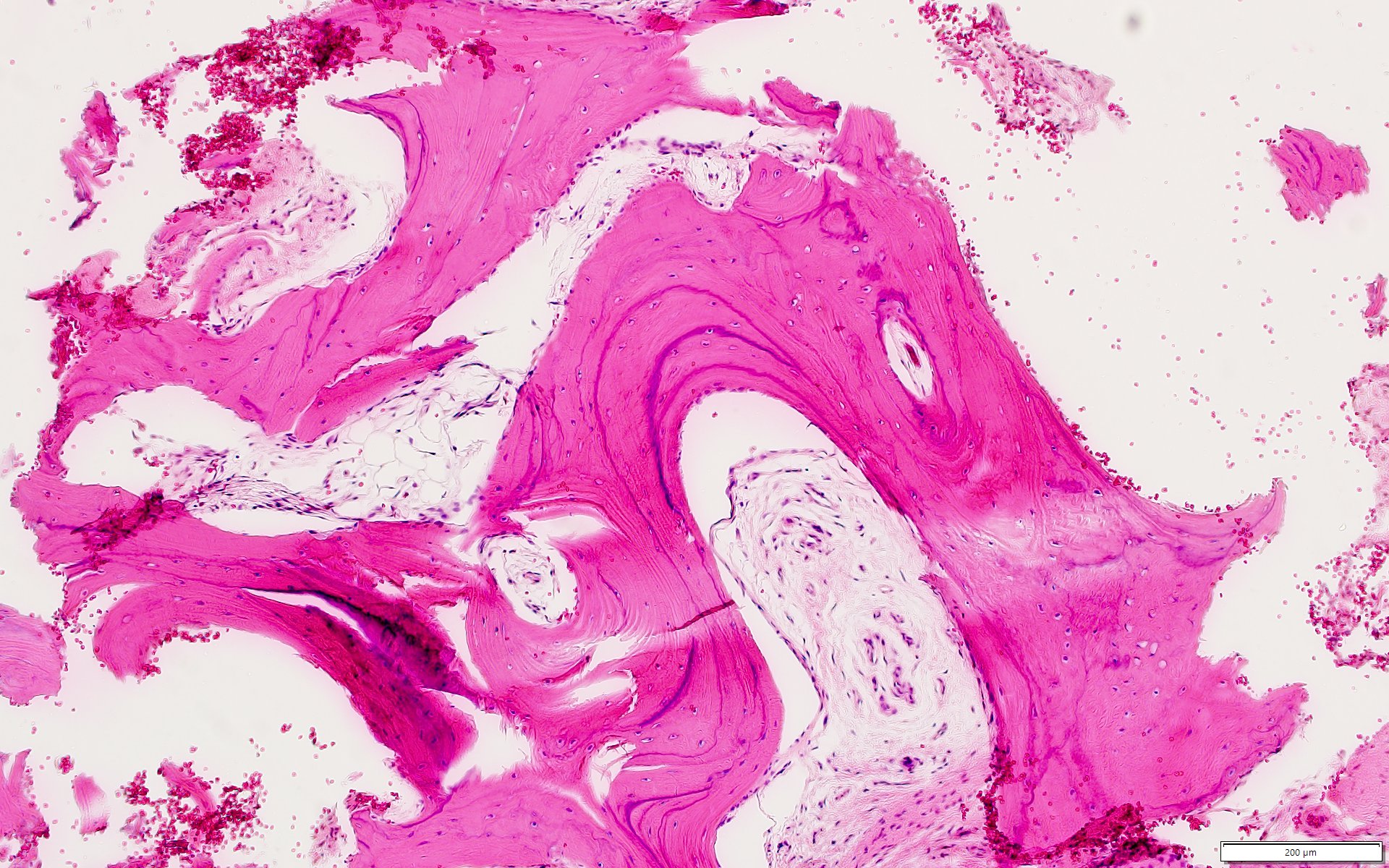
Microscopic (histologic) description
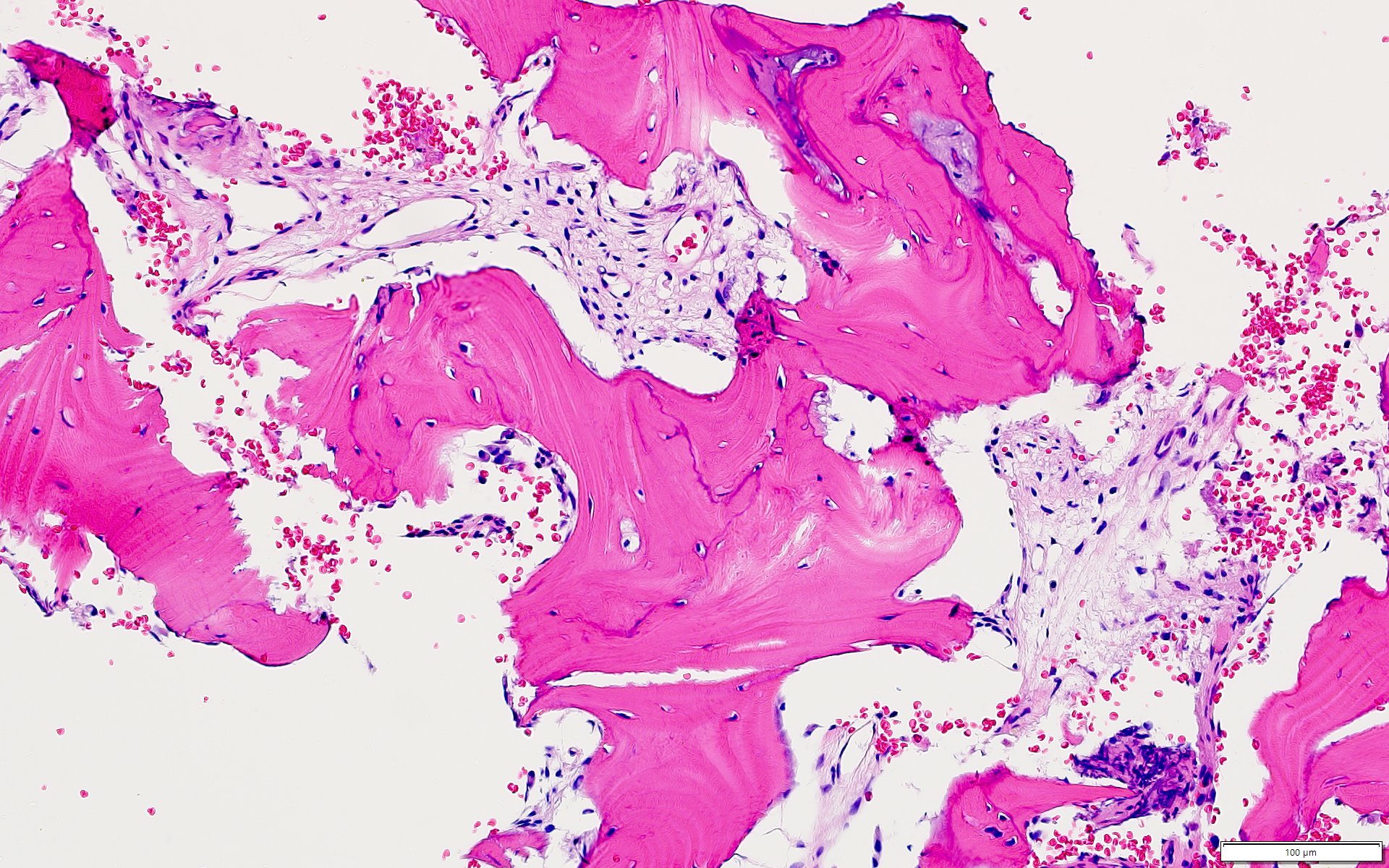
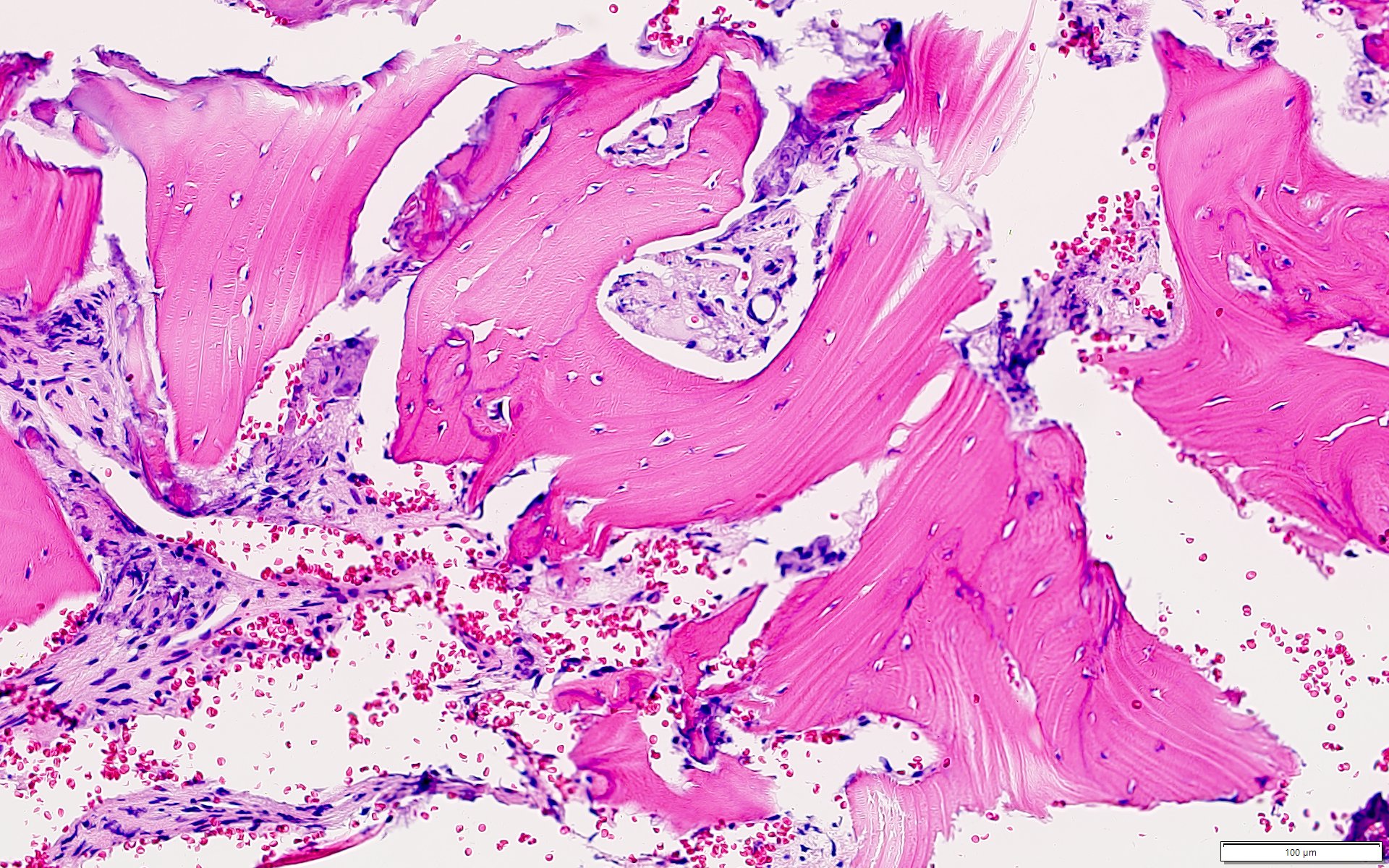
- Replacement of cancellous bone with compact bone (J Endod 2013;39:977)
- Scant fibrous tissue (J Mass Dent Soc 2003;52:52)
- Often no obvious inflammation (J Endod 2013;39:977, J Mass Dent Soc 2003;52:52)
Microscopic (histologic) images
Positive stains
- Morphologic and clinical diagnosis, no stains needed
Negative stains
- Morphologic and clinical diagnosis, no stains needed
Sample pathology report
- Mandible, partial mandibulectomy:
- Sclerotic bone consistent with condensing osteitis
Differential diagnosis
- Idiopathic sclerosis:
- Not inflammatory or neoplastic
- Intraosseous radiopacity of noninflammatory trabecular bone
- Cemento-osseous dysplasia:
- May demonstrate multiple foci
- Cellular fibrovascular connective tissue with mixture of bone and cementum-like particles
- Radiographically characterized by radiolucency or radiopacity surrounded by radiolucency
- Osteoma:
- May be associated with Gardner syndrome, particularly when multiple
- Demonstrates expansion / growth over time with possible displacement of teeth
- No association with inflammation
Additional references
Board review style question #1
Board review style answer #1
D. Radiopaque lesion. Condensing osteitis is most often seen on panoramic Xray as a radiopaque lesion. There is always a lesion identified as it is how the diagnosis is made. Radiolucent lesions include other cysts such as odontogenic keratocyst, dentigerous cyst or periapical cyst.
Comment Here
Reference: Condensing osteitis
Comment Here
Reference: Condensing osteitis
Board review style question #2
What is the most common histologic finding in condensing osteitis?
- Acute osteomyelitis
- Compact / sclerotic bone
- Marked chronic inflammatory infiltrate
- Replacement of bone by fibrous tissue
Board review style answer #2
B. Compact / sclerotic bone. Condensing osteitis is related to chronic inflammation causing sclerotic bone formation. Acute osteomyelitis will not be seen as this is a chronic process. There also will not be a chronic inflammatory infiltrate given the chronicity of the process. There is scant fibrous tissue in this process; it is a reactive boney process.
Comment Here
Reference: Condensing osteitis
Comment Here
Reference: Condensing osteitis