Osteitis pubis is a condition characterized by inflammation of the pubic symphysis, which is the joint located at the front of the pelvis where the left and right pubic bones meet. The condition is typically caused by overuse or injury, and it can result in pain and stiffness in the pelvic area, as well as difficulty walking or moving the legs. Treatment options include rest, physical therapy, and medication to manage pain and inflammation. In severe cases, surgery may be necessary.
What cause Osteitis Pubis
Osteitis pubis is typically caused by overuse or injury to the muscles and ligaments that support the pubic symphysis. The condition is most common in athletes who participate in sports that involve running or kicking, such as soccer, Australian rules football, and hockey. Other factors that can contribute to the development of osteitis pubis include poor conditioning, improper technique, and insufficient warm-up and stretching.
Additionally, it can also be caused by pregnancy, obesity, and certain medical conditions such as osteoarthritis, stress fractures or chronic stress on the pubic symphysis.
It’s important to note that a definitive cause of osteitis pubis may not always be identified.
How to treat Osteitis Pubis
Treatment for osteitis pubis typically begins with conservative measures, such as rest and physical therapy. The goal of treatment is to reduce pain and inflammation, and to strengthen the muscles and ligaments that support the pubic symphysis.
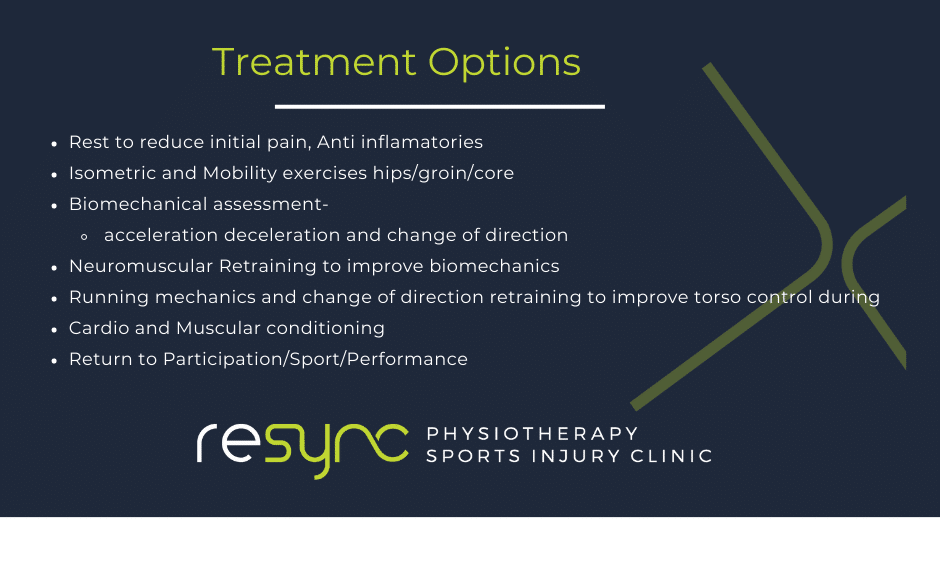
Here are some common treatment options:
- Rest: Avoid activities that cause pain or discomfort and give your body time to heal.
- Physical therapy: A physical therapist can teach you exercises to stretch and strengthen the muscles and ligaments that support the pubic symphysis.
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can help reduce pain and inflammation.
- Injection therapy: corticosteroids can be injected directly into the joint to reduce pain and inflammation.
- Surgery: In severe cases, surgery may be necessary to repair or stabilize the pubic symphysis.
It is also important to address any underlying cause such as obesity, or other medical conditions that may have led to the osteitis pubis.
It’s important to consult a doctor or physiotherapist to properly diagnose and create a treatment plan tailored to your specific case.
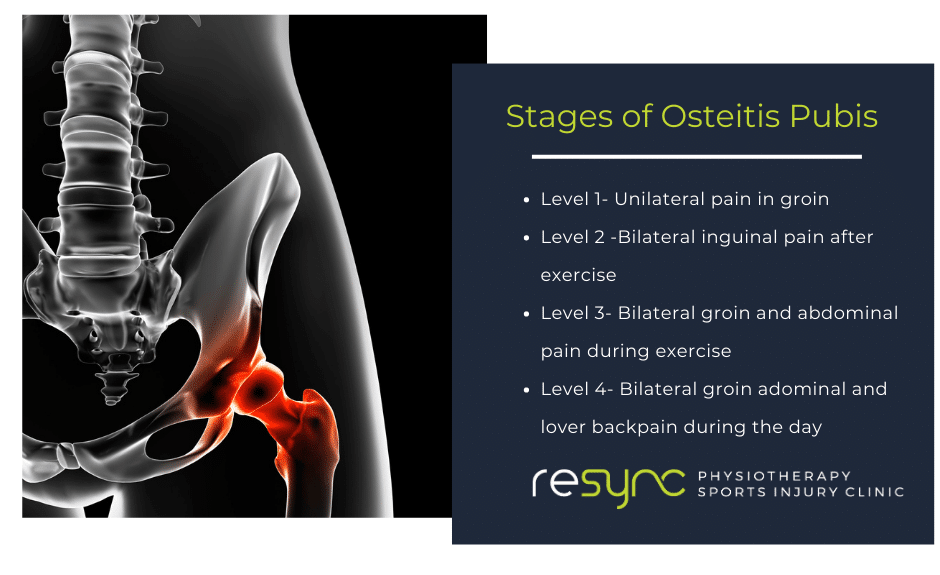
What are the stages of Osteitis Pubis?
Osteitis pubis is typically divided into three stages, based on the severity of symptoms and the degree of inflammation in the pubic symphysis:
- Acute stage: This is the initial stage of the condition, characterized by sudden onset of pain and inflammation. Symptoms may include sharp pain in the pelvic area, difficulty walking or moving the legs, and stiffness in the lower back and hips.
- Subacute stage: This stage is characterized by a gradual worsening of symptoms, as the inflammation and pain continue to persist. Symptoms may include a dull, aching pain in the pelvic area, weakness in the muscles of the lower abdomen, and difficulty sleeping due to pain.
- Chronic stage: This is the final stage of osteitis pubis, characterized by persistent pain and stiffness in the pelvic area, as well as muscle weakness and fatigue. The symptoms may be severe enough to affect daily activities, and may lead to chronic pain.
It’s important to note that osteitis pubis is a progressive condition and if left untreated, it will progress through these stages. Early diagnosis and treatment are crucial to prevent the condition from worsening.
Osteitis pubis in Female vs Male
Both male and female athletes can develop osteitis pubis, however, the condition is more common in males. This may be due to the fact that sports that involve running or kicking, such as soccer and Australian rules football, are more commonly played by males.
Additionally, pregnancy can also cause osteitis pubis in females. The hormonal changes during pregnancy can make the pelvic ligaments and the pubic symphysis more lax, which can put extra stress on the joint and cause inflammation.
Symptoms of osteitis pubis in females and males are similar, with pain and stiffness in the pelvic area being the most common. However, as pregnancy is a risk factor for females, it could also cause additional symptoms such as pain in the lower back, hips, and thighs.
It’s important to note that regardless of gender, early diagnosis and treatment are crucial to prevent the condition from worsening and to return to normal activity or sports as soon as possible.
Is it ok to walk with Osteitis Pubis?
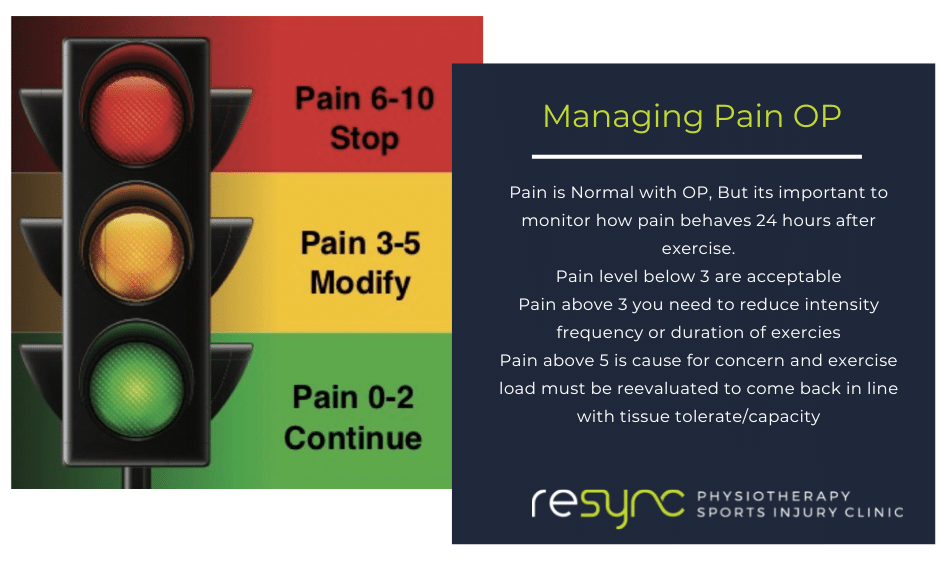
Walking with osteitis pubis can be difficult and painful, as the condition causes inflammation and pain in the pubic symphysis, which is the joint located at the front of the pelvis. However, walking is generally considered to be a non-impact activity, and it can be an important part of the healing process.
During the acute stage of osteitis pubis, it’s important to rest and avoid activities that cause pain or discomfort, to allow the body to heal. However, once the pain subsides and the inflammation is reduced, gentle walking can help to improve circulation, reduce stiffness and help to prevent muscle weakness.
It’s important to consult a physical therapist or sports medicine doctor before starting any exercise program if you have osteitis pubis. They will be able to guide you on the appropriate exercises, and help you to progress safely and gradually.
It’s also important to keep in mind that walking, or any other physical activity, should not cause pain, if it does, it’s important to stop and speak to your doctor or physical therapist.
How long does Osteitis Pubis take to heal?
The length of time it takes for osteitis pubis to heal can vary depending on the severity of the condition and the effectiveness of the treatment. In most cases, the condition can be managed with conservative measures such as rest, physical therapy, and medication, with the healing time ranging from several weeks to several months.
During the acute stage, the pain and inflammation can be severe enough to prevent an individual from participating in their usual activities, and it may take several weeks to several months for the symptoms to subside. In some cases, the pain and inflammation can persist for months or even years, making the condition chronic.
In general, the longer an individual has had the condition, the longer it will take to heal. It is also important to address any underlying cause of the condition such as obesity, or other medical conditions that may have led to the osteitis pubis.
It’s important to consult a doctor or physiotherapist and follow their recommendations to properly diagnose and create a treatment plan tailored to your specific case. With proper treatment, most individuals are able to return to their normal activities.
Exercises for osteitis pubis
Exercise plays an important role in the treatment of osteitis pubis, as it can help to reduce pain and inflammation, and to strengthen the muscles and ligaments that support the pubic symphysis. Here are some exercises that may be recommended by a physical therapist to help treat osteitis pubis:
- Stretching: Gentle stretching exercises can help to reduce stiffness and improve flexibility in the muscles and ligaments that support the pubic symphysis.
- Strengthening: Specific exercises that target the muscles of the lower abdomen, hips and thighs can help to improve the stability and strength of the pubic symphysis.
- Core stability exercises: Exercises that focus on the transversus abdominis, the internal oblique and the multifidus muscles, can help to improve the stability of the pelvis and reduce pain.
- Pelvic tilts: This exercise involves tilting the pelvis backwards and forwards, which can help to stretch and strengthen the muscles of the lower back and hips.
- Pelvic bridges: Lie on your back with your knees bent, lift your hips off the floor and hold for a few seconds, then lower back down.
It’s important to note that these exercises should be performed under the guidance of a physical therapist, to ensure proper technique and to avoid further injury. Also, as the condition improves, the exercises should progress in difficulty and intensity. It’s also important to listen to your body and to stop any exercise that causes pain or discomfort.


